In order to understand this topic it is important to understand the basic anatomy of the spine. Please review the section on basic spine anatomy before reading this section. To understand how the spine works, please review the section on the basic spine biomechanics.
What is a disc herniation?
Vertebrae (back bones) in the spine are separated by a structure called the “intervertebral disc”. These discs act as spacers between the vertebrae and they also function as shock absorbers. Each disc consists of a gel-like center called the “nucleus pulposis”, and a tough outer layer called the “annulus fibrosis”.
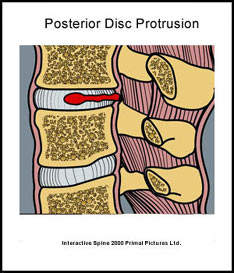
A disc herniation (a.k.a. slipped disc, ruptured disc, torn disc) is the term used to describe an abnormality of the intervertebral disc in which the nucleus pulposis bulges out through the annulus fibrosis.

(Dr. Harry Gouvas, Harrygouvas), Attribution, via Wikimedia Commons
Are there different types of disc herniations?
Disc herniations can vary in severity from isolated tears in the annular fibrosis, to contained nucleus pulposis herniations, disc protrusions, extrusion of the nucleus pulposis (extruded disc) and finally sequestration of the nucleus pulposis or other disc material (sequestrated disc). These terms are most easily explained by the following illustrations:
The term “extruded disc” is used to describe the situation where the nucleus pulposus actually moves outside of the outer fibers of the annulus fibrosis into the spinal canal. The term “sequestered disc” is used to describe the situation where the part of the nucleus pulposus detaches itself from the rest of the disc and ends up inside the spinal canal.
What does a disc herniation feel like?
People with a disc herniation often complain about low back pain. With isolated tears in the annular fibrosis people will often complain of low back pain in the area of the tear. If the protruding disc puts pressure on one of the spinal nerves, the pain may spread to the area that is supplied by the nerve. Depending on which nerve is involved the pain often spreads to the back of the leg or down into the foot. The pain is usually described as a “deep” or “sharp” pain that is aggravated certain positions such as sitting or bending forward at the waist. People with a disc herniation may lean to one side to take pressure off of the herniated disc.
What is sciatica?
Sciatica is the term used to describe pain in the lower back and hip that spreads down the back of the thigh into the leg. It usually occurs as a result of pressure on a spinal nerve from a disc herniation. Disc protrusions, extruded discs and sequestrated discs can all put pressure on spinal nerves. In these cases leg pain may be more common and more significant than back pain.
Where and when do disc herniations occur?
Disc herniations in the lower back usually involve the disc between the fourth and fifth vertebrae (L4-5) or the disc between the fifth vertebra and sacrum (L5-S1). Disc herniations are more likely to occur in adults between the ages of thirty and fifty. During these ages the nucleus pulposis maintains a high water content and is more gel-like. Therefore, it is more likely to move through the injured fibers of the annulus fibrosis. In older people the nucleus pulposis loses water and becomes stiff. As a result it is less gel-like and less likely to move through damaged annular fibers.
How do disc herniations occur?
Disc herniations may be related to one incident, for example, a lifting injury. However, years of improper bending, sitting and poor posture may also cause or contribute to a disc herniation. Over time these activities can cause wear and tear on the annulus fibrosis and eventually the nucleus pulposis can “herniate” through the weakened annulus fibrosis fibers.
Are there any special considerations?
In very few cases a herniated disc may put increased pressure on the nerves that supply the bowel and the bladder. In this case someone with a disc herniation may experience loss of control of their bowels and/or bladder. Numbness and tingling in the saddle area (the area on the inner side of both legs and in between) is also a bad sign as is progressive weakness. It is extremely important that someone having these serious symptoms go to a doctor or the hospital immediately.
How is a disc herniation diagnosed?
The first step in the diagnosis of a herniated disc is to obtain a good medical history and perform a physical examination. X-rays of the lower back may help rule out degenerative disc disease or other bone problems of the spine. An MRI is a very good test to determine if there is a disc herniation. The MRI can detect if there is pressure from the disc herniation on one of the spinal nerves. A CT scan (CAT scan) may also be helpful because it is better than an MRI at looking at the bones in the spine as a cause of pressure on the spinal nerves.
What is the treatment for a disc herniation?
Treatment for a disc herniation should involve a team approach. Most types of treatment for a disc herniation work best when started early. For this reason establishing a correct diagnosis is important. Available treatments include physiotherapy to learn proper movement patterns, education on activity modification, proper posture, and exercises. Physiotherapy may also include traction, manual treatments, and modalities such as gentle electrical currents and heat or ice to help with pain.
Medications may also be an important part of the initial treatment. Doctors may prescribe anti-inflammatory medications, pain medications and/or muscle relaxants. In some cases surgery is required to relieve the pressure the herniated disc is placing on the spinal nerve.
After someone recovers from a disc herniation it is important to maintain a healthy back with proper lifting techniques, proper posture, and exercises to maintain strong stomach and back muscles. These measures will help decrease the chance of another disc herniation. Doctors and Physical Therapists that deal with people with degenerative disc disease can help outline an individualized treatment and recovery program.
What other information is available on disc herniations?
Back Pain Info / Neck Pain Info’s links section has additional information on this topic. Links have been provided to other websites as well as online medical journals. Visit Joint Pain Info. Com for information on other joint injuries and problems.
